Oncothermia which is also known as electro-hyperthermia is a developed treatment designed to overcome the problems of traditional hypothermia by delivering energy to the malignant tissues. The study conducted on a 75-year old patient with non-small-cell lung cancer (NSCLC) presents the outcome of combined oncothermia and radiotherapy. The result of the presented case report suggests that oncothermia combined with radiotherapy may in fact be a promising alternative for advanced-age and/ or frail patients with locally advanced NSCLC.
Hyperthermia enhances the susceptibility of tumors to radiotherapy (RT) and chemotherapy. Oncothermia, also known as electro-hyperthermia, is a new treatment modality developed to overcome the problems of traditional hyperthermia by selectively delivering energy to the malignant tissues. Hyperthermia is an old form of cancer therapy that involves attacking the malignant disease by administering heat in various ways. It has been usually applied as an adjunct to an already established treatment modality; however, medical and technical problems have prevented its wide acceptance. It is suggested that oncothermia, a new concept of hyperthermia, can overcome these shortcomings.
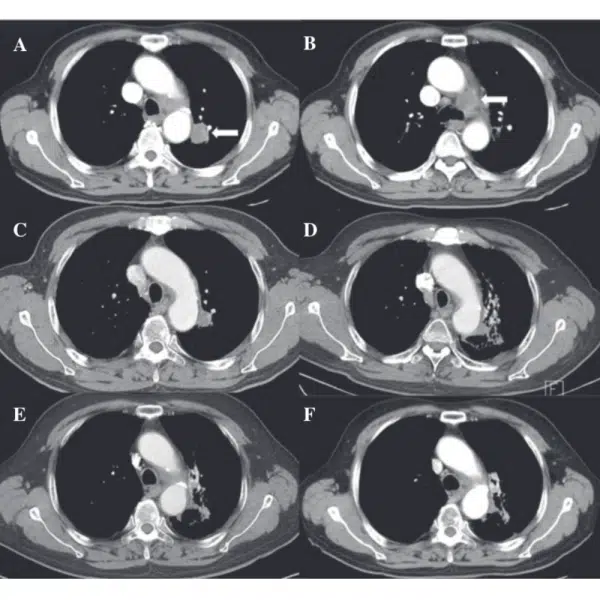
A 75-year-old male an active smoker with a 50-pack-year history. Simple chest radiography showed a mass-like lesion in the left upper lobe. Computed tomography (CT) revealed a 2.6-cm irregular mass with peripheral enhancement in the left upper lobe abutting the descending thoracic aorta. The left lower paratracheal lymph node was enlarged and appeared to have extra nodal extension and recurrent laryngeal nerve invasion.
Pathological examination by percutaneous needle biopsy revealed a poorly differentiated adenocarcinoma. Positron emission tomography-CT showed an increased 18F-fluorodeoxyglucose uptake in both the primary mass and the lymph node. The pretreatment serum level of carcinoembryonic antigen was 2.65 ng/ml. Pulmonary function testing showed a forced expiratory volume in 1 sec of 2.48 liters (78%). A whole-body bone scan, brain magnetic resonance imaging and positron emission tomography- CT showed no evidence of distant metastasis. The TNM clinical stage was determined as T4N2M0 (stage IIIB).
The patient was deemed unfit for chemotherapy due to advanced age and an Eastern Cooperative Oncology Group (ECOG) performance scale score of 2. Definitive RT was scheduled, and the patient agreed to undergo oncothermia concurrently with RT. During the RT simulation, the patient was immobilized in the supine position, with the arms above the head, in a vacuum- bag restriction system. CT was performed using a 16-slice CT scanner and intravenous contrast. Only the gross tumor volume, including the primary lesion and involved lymph node, was included in the RT target; elective nodal irradiation was not considered. A three-dimensional conformal plan was created using the Eclipse treatment planning system 15-MV photons. The RT fractionation scheme was 64.8 Gy in 36 fractions.
RT was performed using a Novalis Tx system. Oncothermia was carried out using the EHY 2000 device. A 30-cm-diameter electrode was applied using the position of the RT simulation target. Oncothermia was performed for 60 min per session, two sessions per week, for a total of 12 sessions. The applied power was gradually and linearly increased from 60 to 140 W, depending on the tolerance of the patient.
Safety and adverse events:
Planned treatments of RT combined with oncothermia were completed without interruption. Acute toxicity was limited to mild odynophagia, which subsided with conservative management. No skin reaction developed. Follow-up CT showed a complete tumor response along with signs of radiation pneumonitis and fibrosis around the treated region; however, the patient developed no specific associated symptoms. There was an improvement in the presenting symptom of hoarseness and the patient was alive without any evidence of the disease at 18 months after treatment.
In conclusion, the present case report suggests that oncothermia combined with radiotherapy (RT), with the former possessing radio sensitizing potential and no additional toxicities, may be a promising alternative for advanced-age and/or frail patients with locally advanced NSCLC.
© 2025 Immucura. All Rights Reserved
Indlæser formular: vent venligst…
Indlæser formular: vent venligst…
Loading form… Please wait…